
The answer could be yes! Skin cancer, the most common cancer, is defined as an abnormal growth of skin cells usually caused by the sun’s harmful rays (UVB and UVA). Like all cancers, they are not contagious, and when caught early skin cancer can be successfully treated. It is estimated that 20% of Americans will get skin cancer in their lifetime, and this number is on the rise. Skin cancers are not hereditary per se, but are higher risk in certain groups of people as will be described below.
The most common forms of skin cancer are:
▪ Basal Cell (BCC)
▪ Squamous Cell (SCC)
▪ Melanoma (aka malignant melanoma)
▪ Actinic Keratosis (pre-cancerous) (AKs)
▪ Dysplastic Nevi (aka abnormal moles, also pre-cancerous)
The last two are mentioned as a precaution, and there are a few others not mentioned in this newsletter which are more rare.
Basal Cell carcinoma is the most common type of skin cancer and usually comes years after sun exposure; the areas affected are typically the most exposed like the head neck and arms. Squamous Cell carcinoma is the 2nd most common and occurs in the same areas, but also on the ears, back and chest. Both types are a risk to people with fair skin, light-colored hair/eyes, but it should be noted that they can occur in anyone with any skin color. These two types are the least invasive and least likely to spread (or metastasize) to organs beyond the skin. The lesions appear as small raised/thickened and discolored (light or dark) bumps that often ulcerate, crust, bleed and act like a sore that won’t heal; when left untreated they may get big.
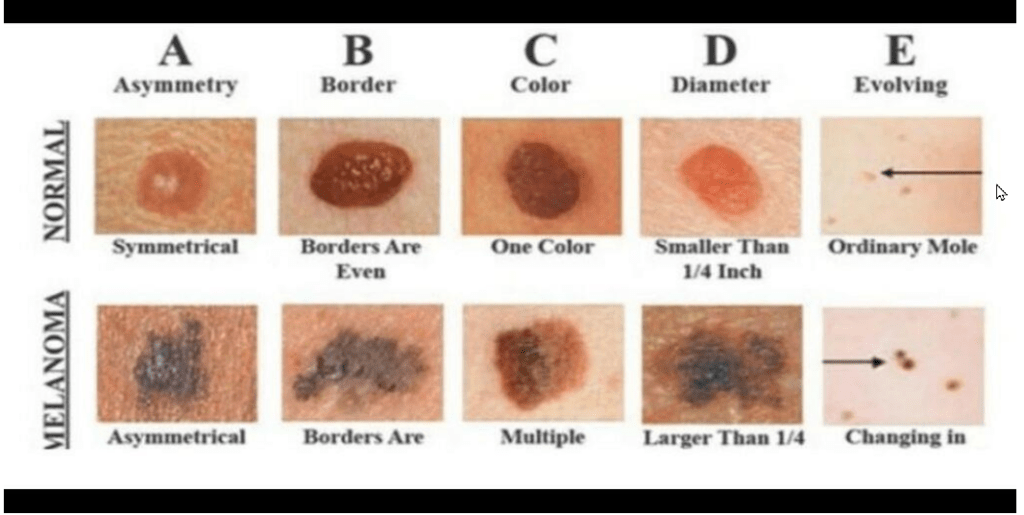
Melanoma develops nearby and/or looking like a mole. It can be present anywhere on the body, but is most commonly on the upper back, chest, lower legs, head and neck. It can spread to the lymph nodes and on to other organ systems more readily than BCC and SCC. Close observation of any mole you have is essential to preventing widespread disease, which will be more difficult to treat and can lead to death. The appearance of melanoma is categorized by ABCDE:
▪ A for asymmetrical, an uneven circle
▪ B for border irregularity, jagged, notched or blurred
▪ C for color difference from the surrounding moles or area
▪ D for diameter, usually more than 6mm (the size of a pencil eraser)
▪ E for evolving, a mole that is changing in shape, size or color
The key to early diagnosis is self-examination on a regular basis! Check yourself (and help a close friend) upon inspection of your skin. Be mindful that the areas mentioned above may not be the only areas affected; some surprising places are the scalp, palms and soles, nailbeds, lips, groin and eyelids. Regarding tattoos, they do not cause skin cancer but definitely can make skin lesions harder to detect.
A common misconception is that people of color are not at risk for skin cancer, that it is not a concern for us. While there are protective factors in the melanin (melanocytes) in colored skin, this is not immunity, or permission to ignore the advice on skin inspection, prevention and seeking medical advice. Late diagnosis and treatment can be dangerous and has led to proportionately higher death rates in this population. Also, the lesions are not easily visible on darker skin, which is even more reason to be vigilant and proactive.
Actinic Keratosis are precancerous growths on the skin that has been to exposed to the sun and UV rays from tanning booths over many years. These can occur in people before age 40 so everybody needs to be cautious about exposure. The lesions are not obvious; dry, scaly and pink or reddish areas, usually on the face and back of the hands, may look like age spots. An extreme example is an actual horn protruding from the skin surface. AKs are precursors to SCC, so any suspicion should be evaluated by a dermatologist for indicated treatment and/or removal.
Dysplastic moles are precancerous and can develop into melanoma, therefore they should be removed as well. They look different from and standout as abnormal amongst other normal moles. If there is any doubt, take a photo and see a dermatologist. A biopsy (small sample of the mole) will be examined under the microscope for any abnormal cellular structure.
Risk Factors—People with light or fair skin, especially with freckles, who sunburn easily; people with light eyes and hair; people with discoloring skin diseases like albinism; people with a history of skin cancer (or family history) or history of severe sunburn; people with burns not related to sunburns; and with multiple moles. This being said, everyone is really at risk and should follow the prevention tips.
Prevention—The best way to prevent skin cancer is to limit sun exposure and avoid the most intense rays between 10am and 4pm, depending on where you live. Obviously, everyone can’t or doesn’t want to do this, so applying sunscreen daily with a “sun protectant factor” (SPF) of at least 30, helps significantly. Make sure the product is waterproof and says broad-spectrum, which means it protects from UVA (aging damage) as well as UVB rays (burning rays.) Check the labels and familiarize yourself with the ingredients.
And the inconvenient news is the sunscreen must be reapplied every hour to 90 mins when you are outdoors and exposed. Sunscreen works best when it is slathered on, so the folks you see with it on their faces are doing it correctly! Wear a hat and light clothing, which offer some protection, and now there is clothing with UPF (Ultraviolet Protection Factor) which has been tested and rated, the higher the number the better. Do not use tanning beds or booths.
Treatment—The first step is to establish exactly what a particular suspicious bump, mole or concerning area is; this is done with examination by a board-certified Dermatologist and biopsy, if indicated. A biopsy is usually accomplished in the office setting. When the results come back from the lab, a treatment plan is developed by the doctor and is unique to the presentation and diagnosis of the lesion. It may involve a wide excision of the skin, which means cutting tissue beyond the edges of the affected area (this is called the “margin”.) There are many other methods of treatment beyond the scope of this discussion, but the important point is to see a professional early and follow the recommendations. It is also imperative to double down on preventative measures if you are diagnosed with any precursor, or actual skin cancer.
Respectfully submitted by Dr. Lan Hodges
References
www.myclevelandclinic.org
www.americanacademyofdermatology.org
www.webmd.com/melanoma
www.pmc.ncbi.nlm.nih.gov/articles
